3D Bioprinter for next generation of "bottom-up" tissue engineering
3D Bioprinter for next generation of "bottom-up" tissue engineering Fraunhofer USA CMI worked under funding from Fraunhofer-Gesellschaft on this project at the interface of engineering and life sciences to design and implement a novel hydrogel-based bioink embedded with mammalian cells, a 3D bioprinter, and automation software.
 |
 |
 |
Objective
The list of patients in dire need of organ transplants grows longer every day. Patients who are fortunate enough to find a 'match' still struggle with immunosuppressive therapy and ultimate organ failure. The goal of 3D bioprinting is to precisely place cells in environments that trigger their growth into fully functional tissues and organs. Fraunhofer USA CMI, and others involved in this effort, are working towards the ultimate goal of bioprinting the patient's own cells into a new and healthy replacement organ.
Methodology
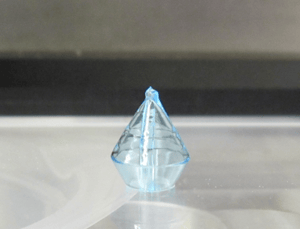
Fraunhofer USA CMI's latest achievement in this field, was the development of a three-dimensional (3D) bioprinting system capable of multimaterial and multiscale deposition to enable the next generation of "bottom-up" tissue engineering. This area of research resides at the interface of engineering and life sciences, requiring an interdisciplinary team of engineers and scientists.
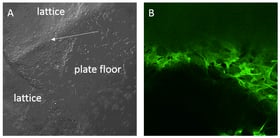
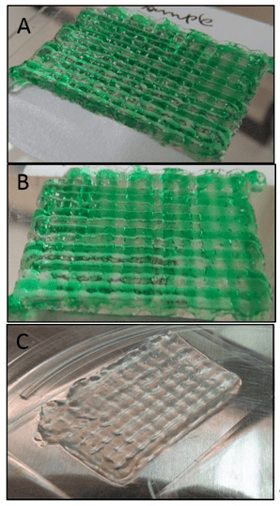
Fraunhofer USA CMI's bioprinter has three components uniquely combined into a comprehensive tool: syringe pumps connected to a selector valve that allow precise application of up to five different materials with varying viscosities and chemistries, a high velocity/high-precision x–y–z stage to accommodate the most rapid speeds allowable by the printed materials, and temperature control of the bioink reservoirs, lines, and printing environment.
Results
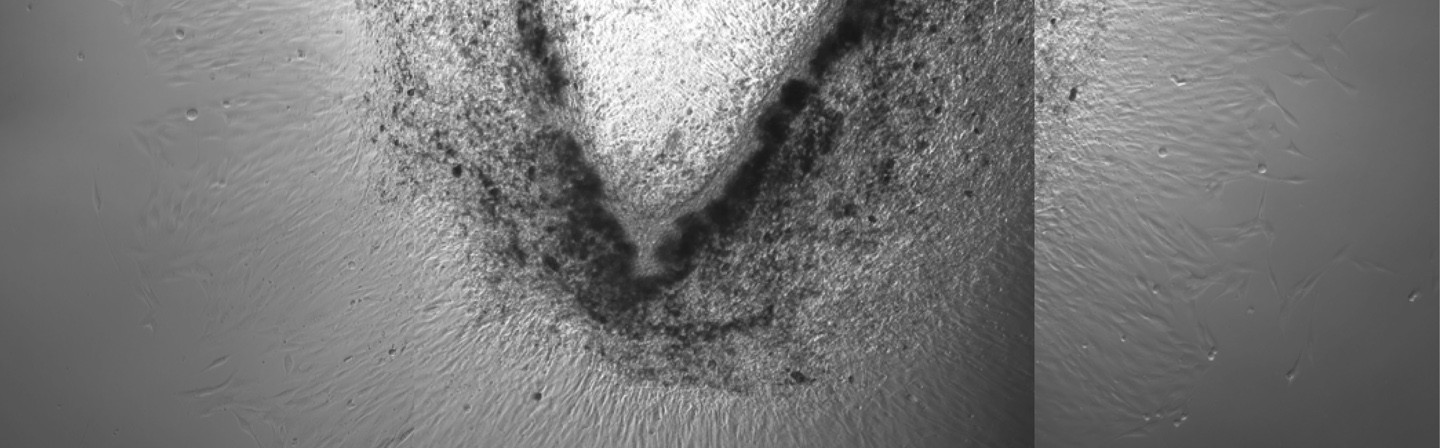
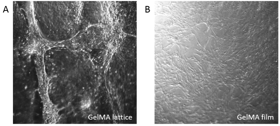
Fraunhofer USA CMI’s custom-designed bioprinter is able to print multiple materials (or multiple cell types in the same material) concurrently with various feature sizes (100 μm–1 mm wide; 100 μm–1 cm high). One of these materials is a biocompatible, printable bioink that has been used to test for cell survival within the hydrogel following printing. Hand-printed (HP) controls show that our bioprinter does not adversely affect the viability of the printed cells.
Collaborators / Funding
This project is funded by Fraunhofer USA. New applications of the bioprinter to improve the osseointegration of hip implants is funded by Fraunhofer-Gesellschaft and carried out by Fraunhofer USA CMI, Fraunhofer IGB and Fraunhofer IAP.
Future Directions
The researchers at Fraunhofer USA CMI are currently focused on improving osseointegration of hip implants and have successfully bioprinted scaffolds that support differentiation of bone cells.
Publication
Fraunhofer USA CMI reports the design and build of the 3D bioprinter, the optimization of the bioink, and the stability and viability of the printed constructs in their publication:
Campbell J, McGuinness I, Wirz H, Sharon A, Sauer-Budge AF. Multi-material and Multi-scale Three-dimensional Bioprinter. J. Nanotechnol. Eng. Med. 2015; 6 (2):021005. DOI: 10.1115/1.4031230.